Traditional clinical trial design in oncology of grouping together patients based on their cancer type has a high attrition rate, with an estimated 95% of potential anticancer drugs failing during development. Researchers are constantly working on ways to overcome this, and one method which is gaining popularity is a “basket” study, grouping together patients by mutation type rather than disease.
When a clinical trial fails there is sometimes anecdotal evidence about “exceptional responders” – one patient or a small number of patients who responded exceptionally well to the novel treatment. Now, following a failed trial, instead of scrapping an agent next generation sequencing is being used to see if these exceptional responders could hold the key to predicting subgroup response. One well-cited example of this is an everolimus trial (an mTOR inhibitor) in metastatic bladder cancer. Overall, everolimus did not hit the primary endpoint (improvement in progression free survival); however, there was some individual patient response with one particular patient having a complete response for more than 4 years. Whole genome sequencing revealed that the patient had a specific loss-of-function mutation in a tumor suppressor gene (TSC1) that activated mTOR. Three other patients with this TSC1 mutation had partial responses to everolimus, suggesting the mutation correlated with sensitivity to the drug. Even though this hypothesis was based on a small number of patients, the data was enough to prompt a full clinical trial of everolimus in TSC1-mutant cancers.
The example above highlights the concept of a basket study – to identify a mutation that causes a clinical response to a specific agent, and then to enroll all patients with the mutation into a clinical trial regardless of their cancer type. Basket trials look to enroll at least 10 to 15 subjects per cancer type, putting each cancer in its own separate study arm or “basket” in the trial. Each arm/cancer type can then be analyzed separately for response, as well as the overall study population being assessed as a whole. This type of phenotype-to-genotype trial is particularly useful when a mutation or cancer type is rare, the studies usually include an arm for “other” which is used for patients who have the mutation of interest in a rare, or never before seen, cancer type. These diseases are particularly difficult to plan clinical trials for individually, due to the small number of target patients.
Basket studies are increasing in popularity, reflecting a growing confidence that sequencing and molecular diagnostics can predict treatment response. One of the main problems now is to find patients for basket trials. The US National Cancer Institute along with academic medical centers such as Memorial Sloan Kettering Cancer Center and the Dana-Farber Cancer Institute are collecting samples from exceptional responders for sequencing, with the aim of creating a national database of the responders and their mutations. So far, around 100 exceptional responders have been identified from 10 years of clinical trial research. Memorial Sloan Kettering Cancer Center has also committed to screening every patient with metastatic disease in the next 12 months (estimated to be 10,000 to 12,000 patients) for somatic mutations, to identify driver alterations and germline variants that could contribute to cancer initiation
One problem further down the line may be FDA approval from basket studies – while the FDA is now approving agents from clinical study data involving smaller numbers of patients it is not likely to approve a drug based on data from only a few subjects. Where agents are shown to work, studies may need to expand around one specific arm, or further follow up studies may need to be run. Currently, the FDA usually approve agents based around a cancer type rather than a molecular target; however, there is nothing stated in the regulations to say this has to be the case. It is thought that with solid data, showing effective and safe treatments from well-run trials, that the FDA would welcome this new trial type.
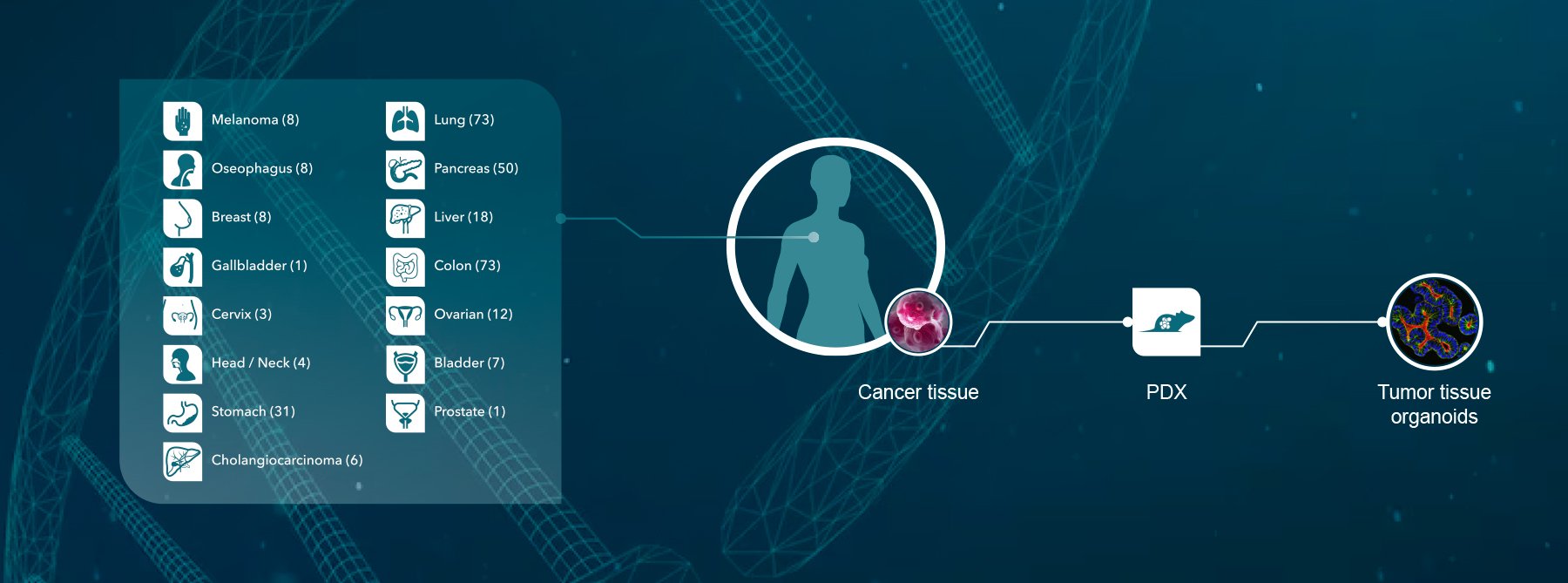
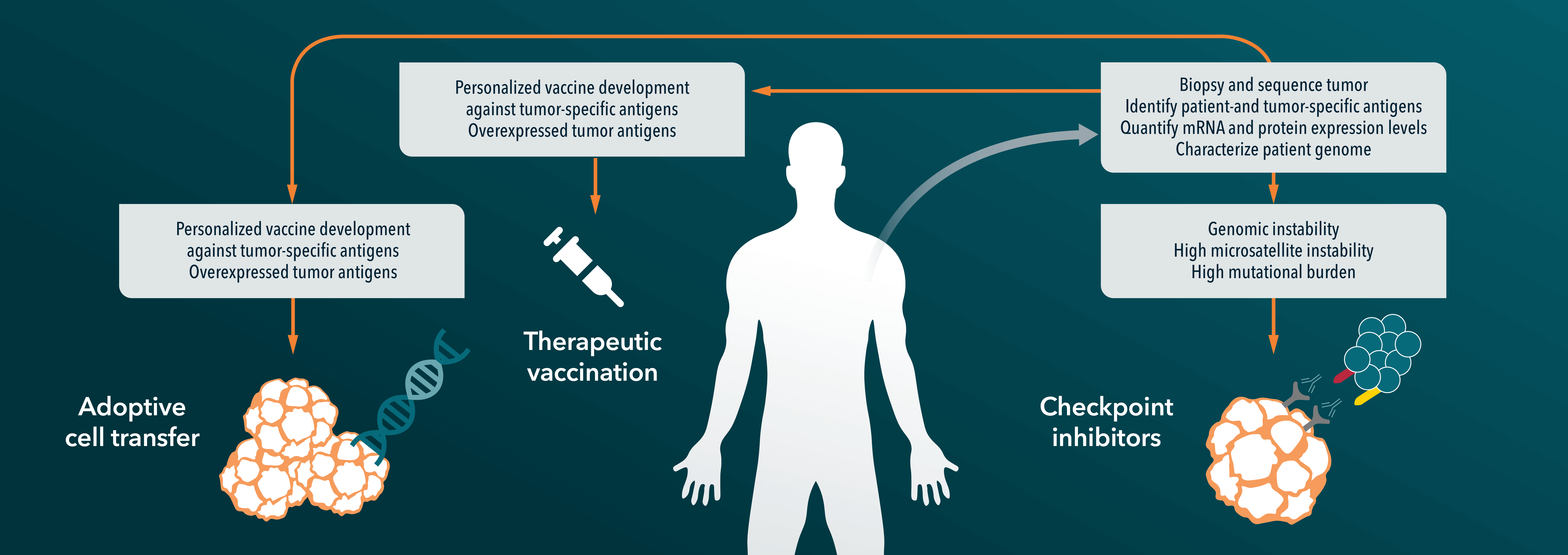
Crown Bioscience can help in defining your basket study or in identifying potential exceptional responders. We utilize the world’s largest commercial collection of >1000 genomically characterized PDX models (large enough to be truly reflective of the patient population) to run HuTrials™, preclinical Phase-II like trials to evaluate your oncology agents. Using bioinformatics and biostatistical analysis of model responders and non-responders, we identify a HuSignature™ from your results – a specific genetic signature which has a high correlation with drug response or drug resistance, and which can be used to identify potential exceptional responders in the clinic.
Contact us at busdev@crownbio.com to talk to our experts about how HuTrials and HuSignature can drive forward your basket study today.