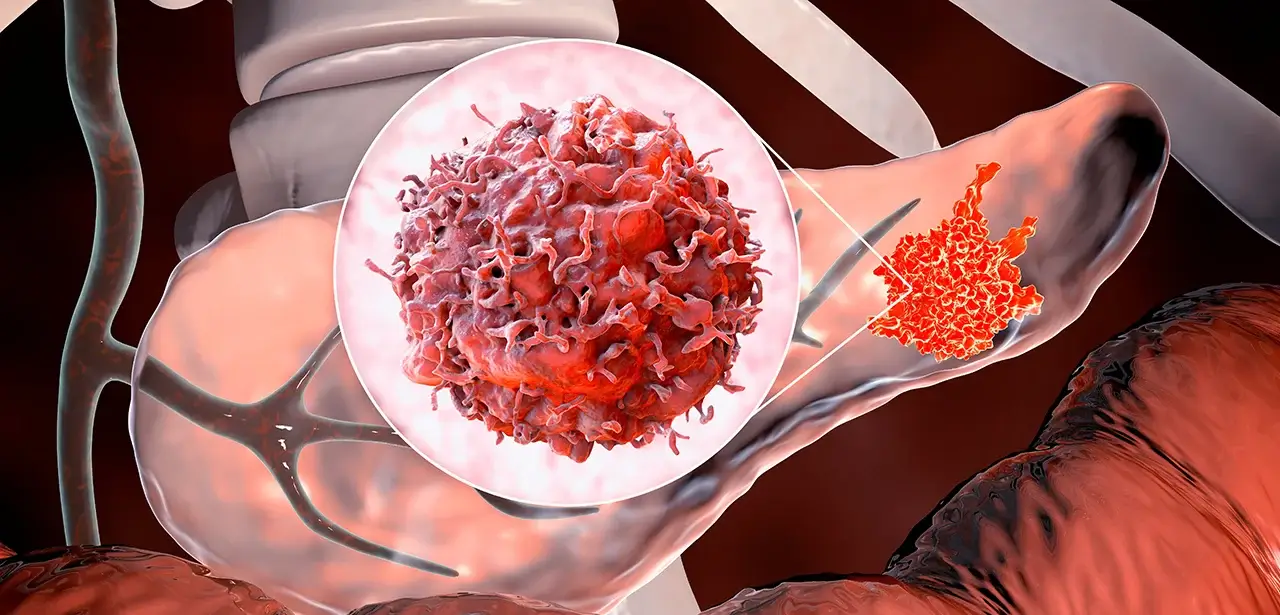
Pancreatic cancer is usually diagnosed at a late stage, which has resulted in the disease having particularly poor survival rates around the world. Finding methods to allow earlier detection and treatment could massively improve patient survival, and are a hot research topic in the field. A recent study investigating altered metabolism in pancreatic adenocarcinoma patients could now have found an early warning marker that might go on to be useful in screening for the disease.
Pancreatic cancer accounts for only around 3% of all cancers in the US, but for 7% of cancer deaths. The disease has low survival rates – in 2014 around 46,000 people will be diagnosed with pancreatic cancer in the US, and only around 7% of these people will survive the disease. The most common form of pancreatic cancer is pancreatic ductal adenocarcinoma (PDAC), which has few early symptoms, and results in most patients being diagnosed at an advanced stage. This makes a massive contribution to the poor survival rates, with many patients dying within one year of their diagnosis. This outlook is repeated around the world – in the UK for all adults diagnosed with pancreatic cancer, only 19% live for at least 1 year after diagnosis, 4% for at least 5 years, and 3% for 10 years.
However, the earlier that pancreatic cancer is diagnosed, the higher the survival rate for the disease – if the cancer is caught before spreading outside the pancreas and surgery is possible, then the five year survival rate in the UK increases five-fold to 20%. This has led teams of researchers to investigate how they can improve the early detection of PDAC, with one research team recently publishing their findings in Nature Medicine. The researchers decided to focus their study on altered systemic metabolism which is linked to the development of PDAC. The study investigated circulating metabolites to see whether altered metabolism could be used to understand the processes of early stage PDAC progression, when diagnosis and treatment could really improve patient outcomes.
The team used blood samples from four prospective cohort studies, to compare 100 substances from 1,500 different people who either developed PDAC or who were classed as their matched controls. The researchers found that people who developed PDAC had higher levels of branched-chain amino acids in their blood than people who did not develop the disease. The elevated levels were associated with a greater than two-fold risk of future PDAC development, with the highest risk being several years before diagnosis. It was shown that the increase in branched-chain amino acids was due to the early presence of a pancreatic tumor and its growth, which causes the breakdown of muscle tissue and the release of the branched chain amino acids into the blood. This was confirmed in mouse models with newly formed pancreatic tumors, which also had above normal levels of these amino acids in their blood.
This study shows that the breakdown of muscle protein begins much earlier in the PDAC development process than originally thought, and could in the future potentially be the basis for the early detection of this tumor type. Currently, as a stand-alone test, branched-chain amino acids do not have the sensitivity or specificity necessary to be used as a population screening tool, with further research needed in this area. The study authors suggest that this marker could be used along with other risk factors such as smoking, inherited genetic variants, and other potential circulating markers, to create a risk stratification tool for early patient screening.
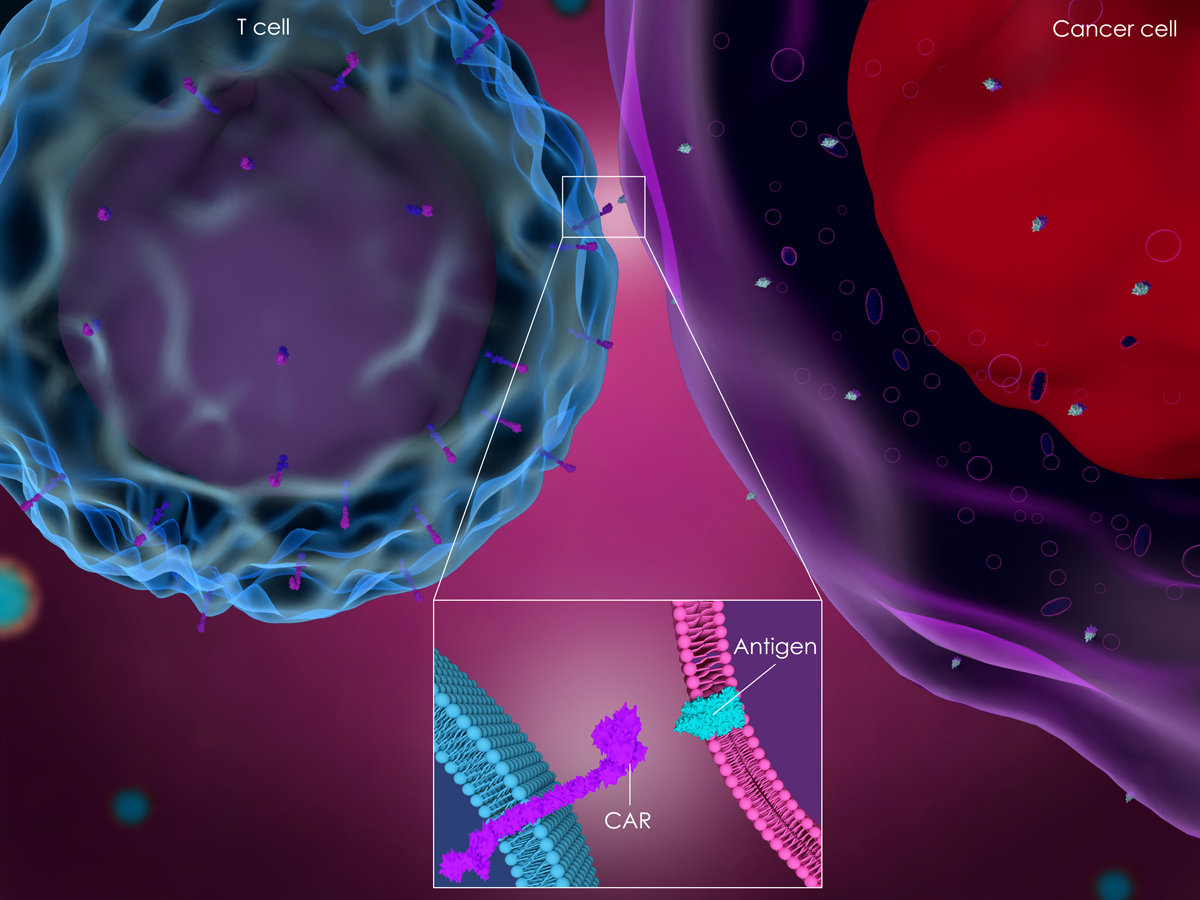
Crown Bioscience support every effort made in improving the early diagnosis of pancreatic cancer, and the enormous survival benefit that it could bring. We support research into pancreatic cancer through the use of our large collection of clinically relevant cell line derived xenograft and patient-derived xenograft (PDX) models available for oncology drug discovery and translational sciences. We have the largest commercially available collection of over 1,100 patient-derived xenograft models (HuPrime®), which contains a large cohort of pancreatic cancer patient-derived xenografts including PDAC models. All HuPrime models are well-characterized and are easily searchable through our free, online database (HuBase™) which can be used to identify relevant models to interrogate biomarkers, pathways, and efficacy. Contact us at busdev@crownbio.com to talk to our experts about how Crown Bioscience can meet your patient-derived xenograft research needs and how we can drive forward your pancreatic cancer research today.