Resistance to chemotherapy is the major factor affecting the survival rate of women who develop high-grade serous ovarian carcinoma (HGSC), the most malignant form of ovarian cancer. New findings could help anticipate which drugs are likely to be ineffective, and could buy some precious time to patients in need.
High-grade serous ovarian carcinoma (HGSC) accounts for 70% of all ovarian cancers and 60% of the ovarian cancer related deaths. Every year, about 80,000 women around the world die of HGSC, and these numbers have barely declined in recent decades, despite continuous medical efforts. Most of ovarian cancer diagnoses respond to chemotherapy at first, but the vast majority relapse due to emergency of chemotherapy resistance.
Researchers from the University of Glasgow and from Melbourne's Peter MacCallum Cancer Centre, led by Professor Grimmond and Professor Bowtell, sequenced the entire genomes of 114 HGSC samples from 92 patients at various stages in disease progression ranging from early diagnosis up until immediately after death and including successfully and unsuccessfully treated cases. This type of analysis offered them the unparalleled portrait of ovarian cancer evolution during the course of treatment and allowed them to find clues about how initially vulnerable cancer cases eventually become highly resistant to chemotherapy.
Beside evidencing the most common genetic alterations occurring in primary ovarian cancer, such as TP53 and BRCA1 mutations, the results published in the journal Nature, show that tumors which become resistant or refractory to treatment, contain increased copy number of CCNE1, a gene responsible for regulating cell division. HGSC that successfully dodged chemotherapy also tend to contain breaks in several tumor suppressor genes, while BRCA1 and BRCA2, commonly mutated in primary tumors, revert back to wild-type restoring cancer cells ability to repair chemotherapy-induced DNA damaged. Other mechanisms of acquired resistance include the increased ability of tumors to pump out chemotherapy drugs via the upregulation of the drug efflux pump MDR1.
Although these pathways to resistance are not novel to oncology researchers, this study emphasize the heterogeneity and apparent adaptability of the HGSC genome under selective pressure by chemotherapy, and indicate that overcoming resistance to conventional chemotherapy will require a diversity of approaches.
An earlier report published on the British Journal of Cancer by researchers at the Queen's University School of Medicine in Canada found 11 genes differently expressed in chemoresistant versus chemosensitive HGSC, the most significant of which was STAT1, a protein involved in pro-inflammatory responses that could, following this discovery, be used as biomarker in HGSC patients to indicates the likelihood that the tumors will respond to chemotherapy. This study confirms the existence of intrinsic drug resistance in HSGC that is governed by both tumour and host factors, and suggests that an activated tumour immune microenvironment could determine a positive response to chemotherapy in HGSC.
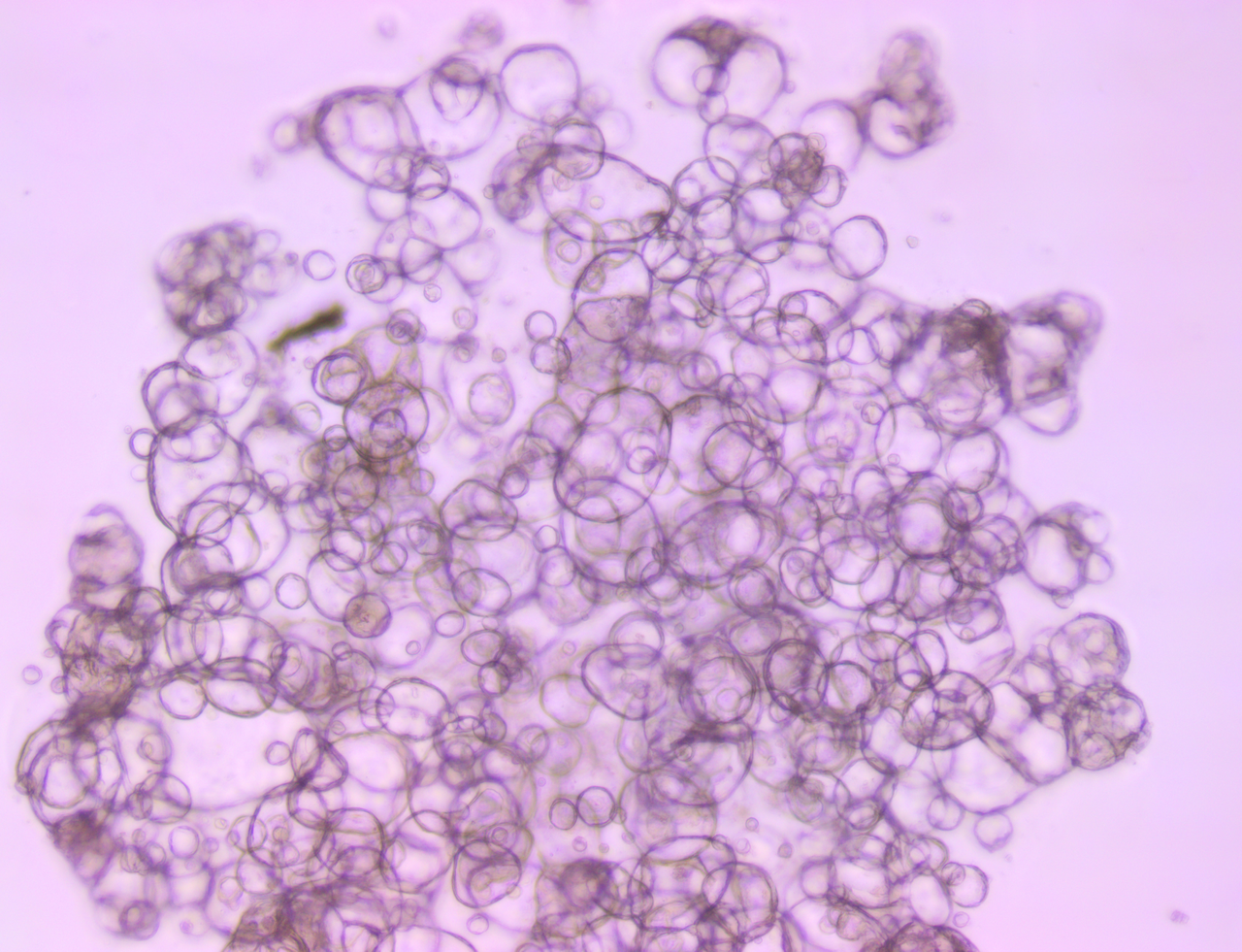
Preclinical models are essential to explore the mechanisms of drug resistance and to provide a fast route from preclinical testing to clinical validation of new compounds. Crown Bioscience has developed several highly predictive ovarian cancer models for preclinical drug evaluation included in our HuPrime® and PDXact™ collections of patients derived xenografts (PDX). Our fully validated and extensively characterized PDX models can be employed in HuTrials™, our surrogate Phase II mouse clinical trials, to identify responder and non-responder populations, gene signatures and predictive biomarkers for patient stratification in the clinic using our HuSignature™ and our HuMark™ translational platforms. Our ovarian cancer services also include syngenic models, GEMM, and MuPrime™ models - allografts of spontaneous murine tumors, studied in fully immunocompetent mice.
Contact us at busdev@crownbio.com to talk to our experts about how Crown Bioscience can drive forward your ovarian cancer research today.