The way we treat cancer is rapidly evolving. Over the years we have learnt that grouping together patients based on their cancer type and then treating them all with the same agent has limited success and leads to incredibly high attrition rates. Researchers are now undertaking a radically different approach in umbrella trials, including the innovative Matrix NSCLC study, dividing patients within a cancer type by the genetic makeup of their tumor and testing multiple treatments in parallel.
With the attrition rate for oncology agents at 95% we need to urgently rethink the way we conduct clinical cancer research. Thanks to the significant leaps forward in molecular medicine we now understand that two cancers that come from the same organ and look the same under the microscope (that display the same tumor pathology) can have different genetic causes, whereas cancer types from different organs can share the same genetic abnormalities. In clinical terms this means that patients with different cancer types can benefit from the same targeted therapy that is specifically tailored to the genetic makeup of their tumor.
This approach has been the focus of “basket trials” that enroll patients across different cancer types with the same abnormality (or biomarker) to all be tested with the same agent. This is in contrast to traditional clinical trials, which usually focus on only one cancer type, and sometimes regardless of mutation status.
Another trial type based on genetic abnormalities, and that is now gaining more coverage is “umbrella” trials. These trials take only one disease type (e.g. lung cancer) but split patients out by their mutations and genetic markers to trial a whole range of therapeutic options in parallel. In an umbrella trial patients with a given molecular makeup of their cancer are assigned to the specific treatment arm that should hopefully result in their maximum response. The trials are designed to be modular and flexible: their arms can be moved in and out of a study according to patient results and when new drugs become available. This flexibility and the great variety of drugs tested at the same time should mean that as many patient groups as possible have their optimum treatment options identified.
Both trials have in common the recognition of the importance of precision profiling of patients to further personalized medicine that translates into finding “the right treatment for the right person at the right time”.
One key umbrella trial trailblazing in the UK is the National Lung Matrix Trial, a master collaborative effort between CRUK, AstraZeneca and Pfizer, who are jointly financing the program with NHS support. Professor Gary Middleton, who is supervising the Matrix trial, presented the concept during the Crown Bioscience first EU symposium on translational oncology held in February and described the study as the “largest ever personalized medicine trial in any cancer”.
The Matrix trial is a multi-drug, multi-arm genetically directed Phase II trial run by the CRUK Clinical Trial Unit at the University of Birmingham that is recruiting NSCLC patients who are Stage IIIb or later. Lung cancer kills around 35,000 people every year in the UK, with NSCLC patients making up 78% of lung cancer diagnosis in England and Wales and new optimized treatment options are rapidly needed to improve survival. For this trial AstraZeneca and Pfizer have opened their archives of drugs to researchers, and up to fourteen different agents could be tested to target very specific mutations in patients with otherwise extremely limited options.
We are delighted to see the evolution of clinical trials towards study types that should find the correct targeted agent for the correct patient groups in the most efficient fashion possible. At Crown Bioscience we recognize that the oncology drug development process is currently highly inefficient and needs a rapid overhaul to reduce attrition rates.
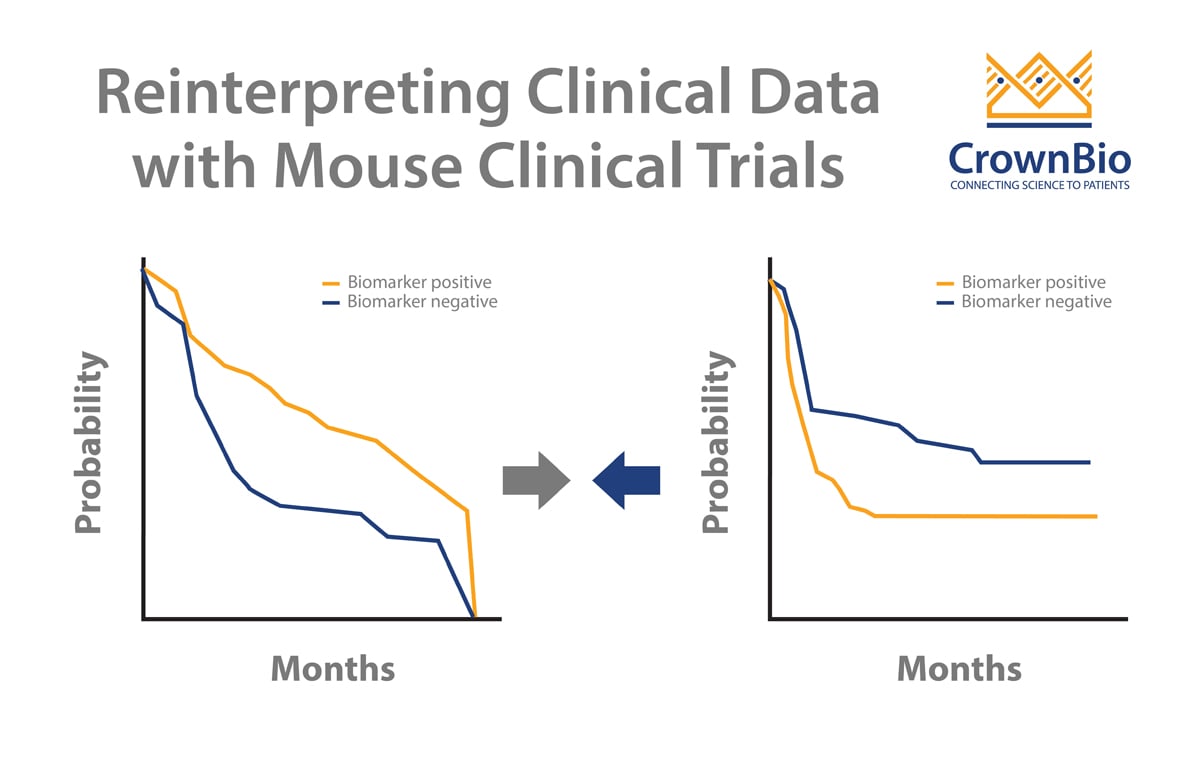
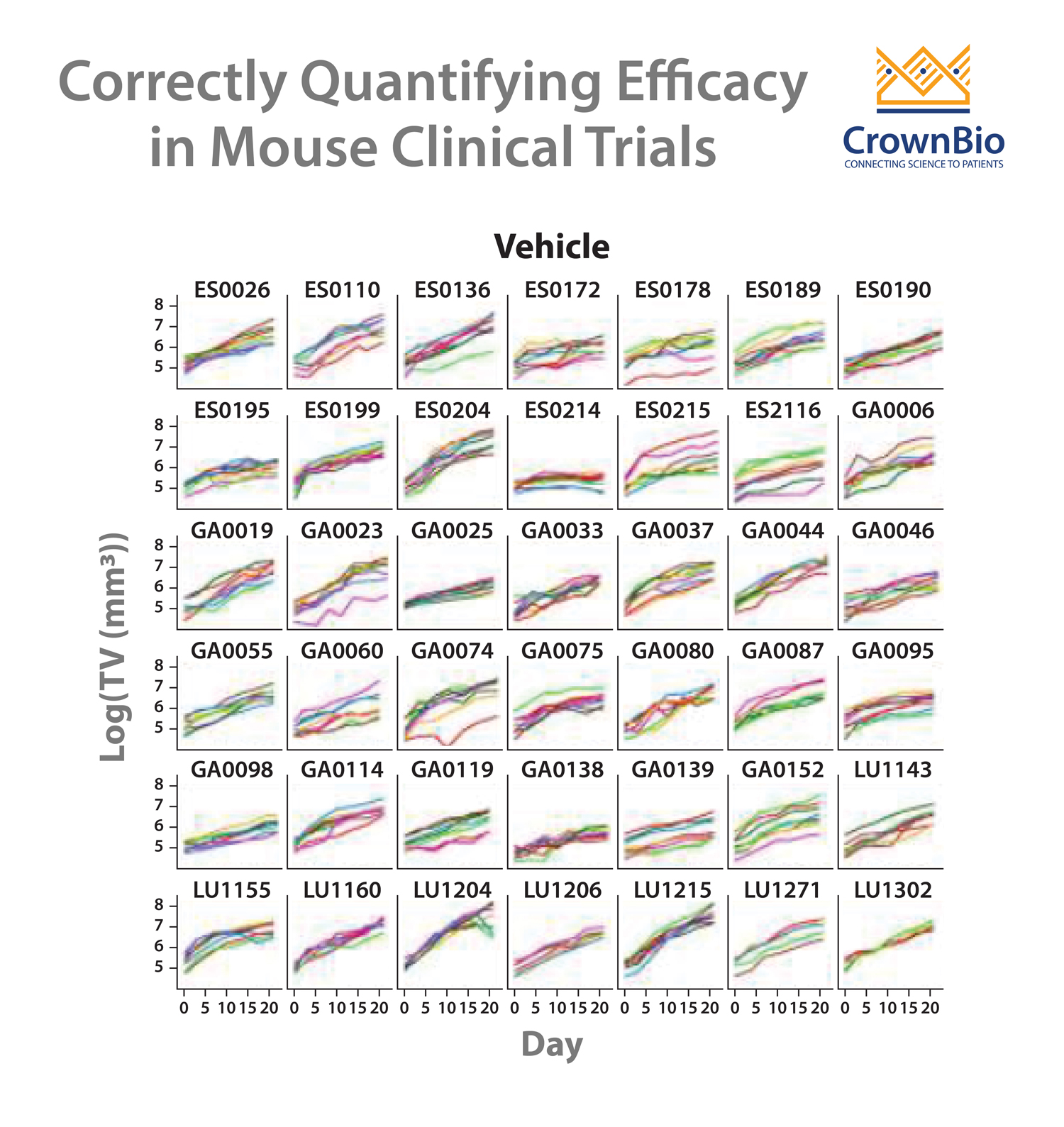
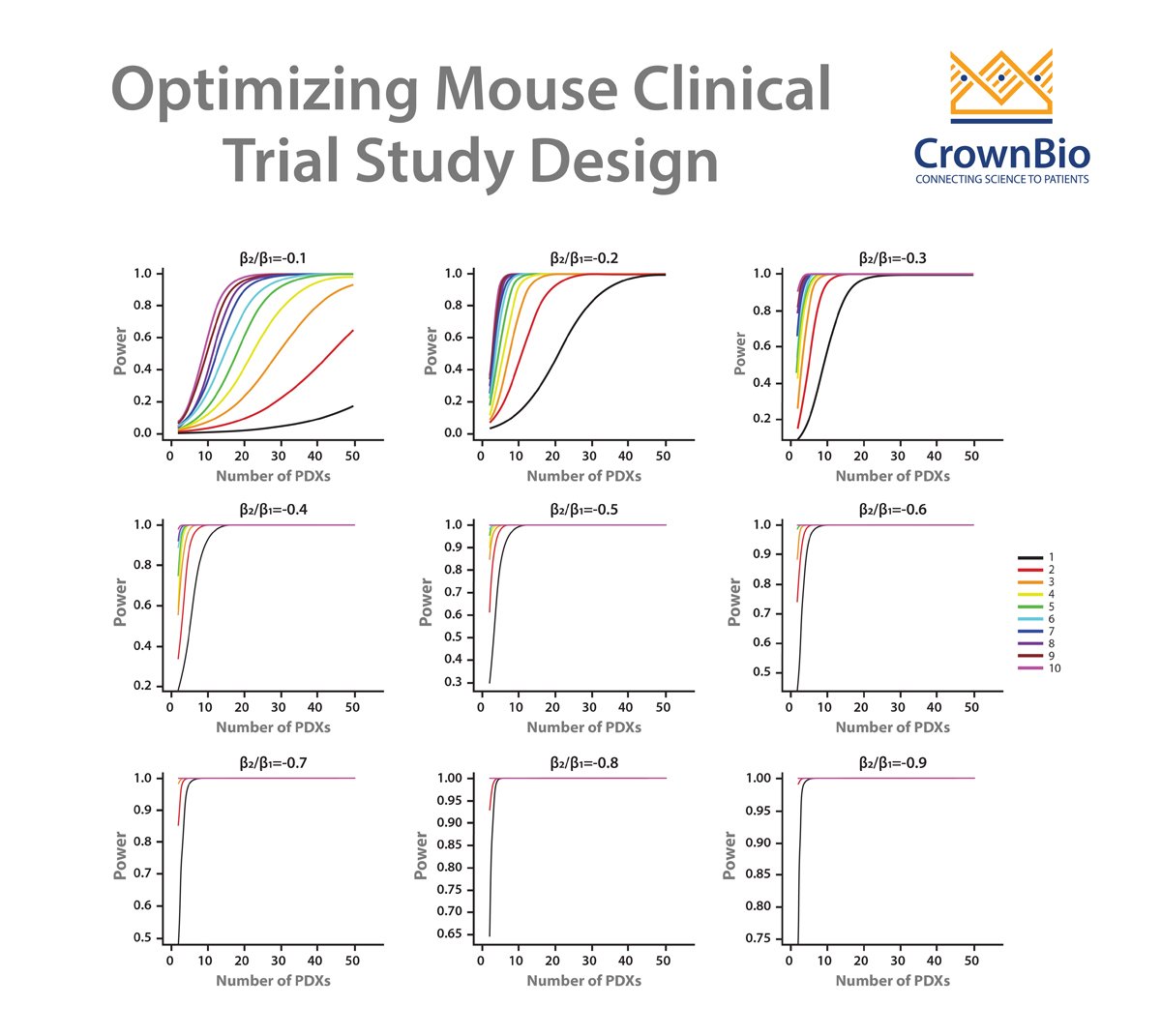
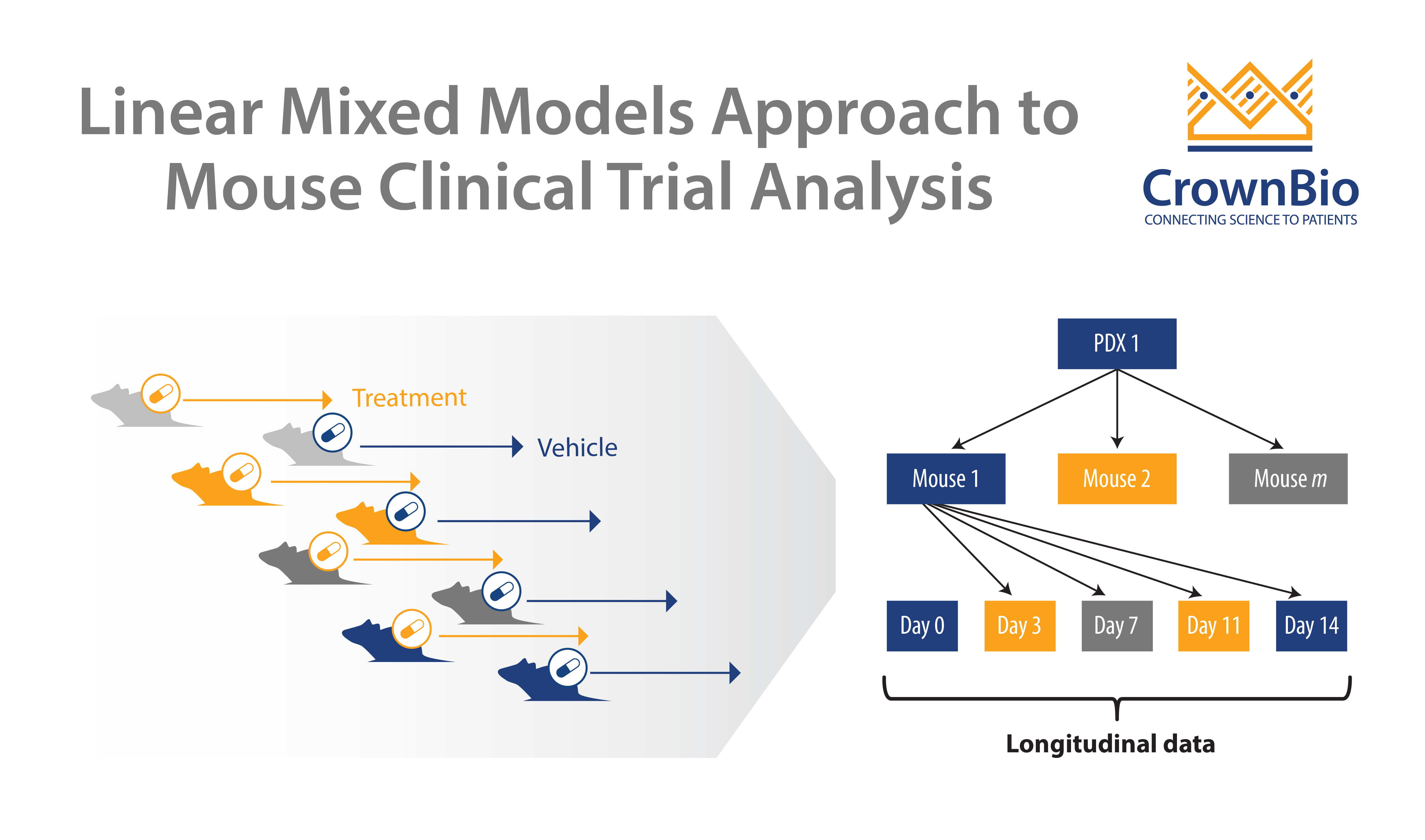
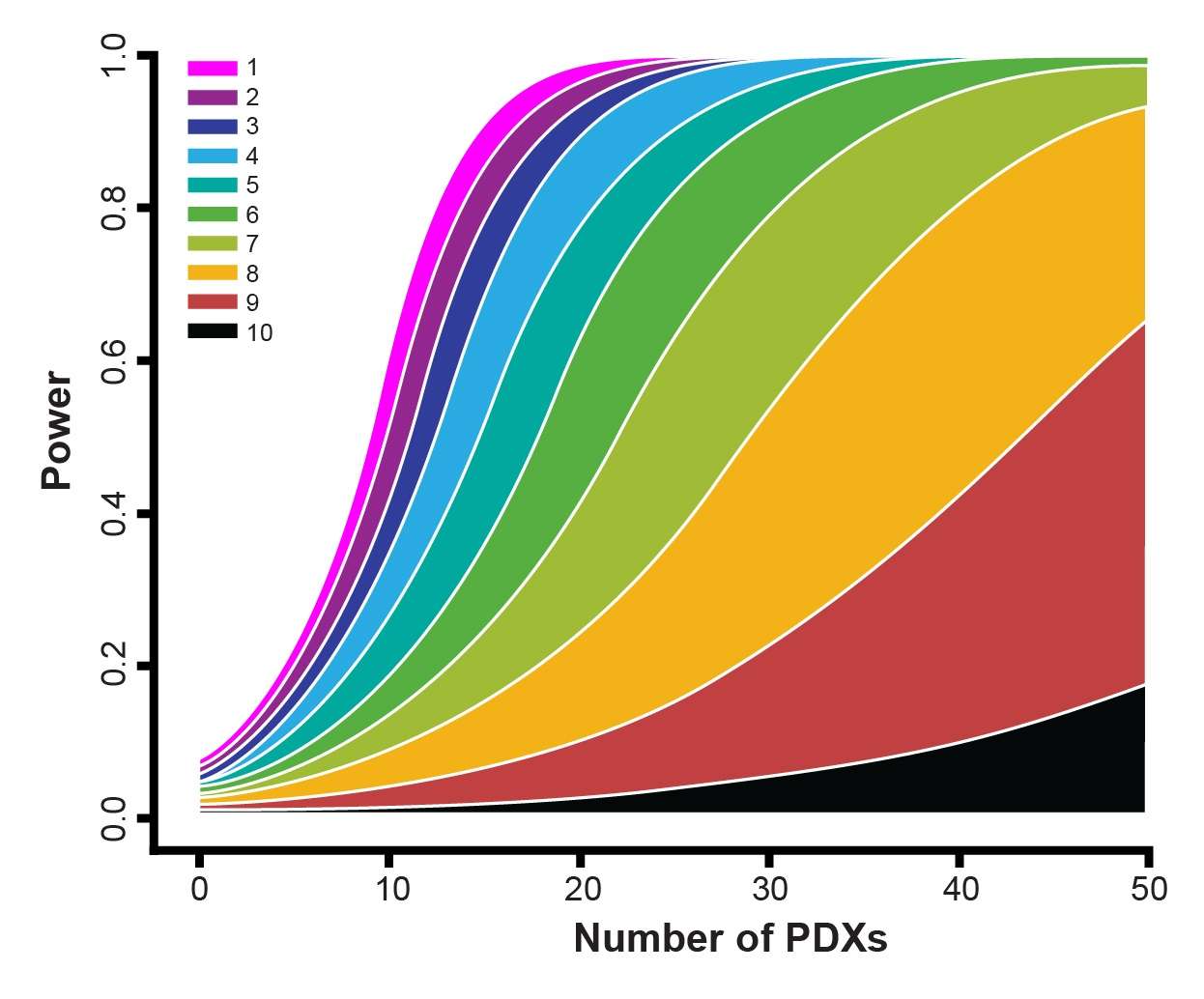
We can help reduce attrition rates and maximize the efficiency of your drug discovery program thanks to the world’s largest commercial collection of >1,600 genomically characterized patient-derived xenograft (PDX) models (HuPrime®; large enough to be truly reflective of the patient population) to run HuTrials™, preclinical Phase-II like, human surrogate trials to evaluate your oncology agents. Combining this with our HuMark™ Translation Platform, which spans a range of experiments and analyses from tissue collection to human surrogate trial data analysis, allows you to predict biomarkers of response to your agent, and help to validate antitumor effects against predicted human targets.
Contact us at busdev@crownbio.com to talk to our experts on how we can further your translational oncology needs through our patient-derived xenograft models and translational oncology resources today.